×
Select Your Country
 International
International

×
Select Your Country
 International
International

It is an intricate yet life-saving surgical technique known as a Whipple surgery (also known as a pancreaticoduodenectomy) is used to treat pancreatic cancer as well as other diseases and abnormalities of the pancreas, bile duct, duodenum, and other organs. The surgery entails the removal of the duodenum, bile duct, a section of the pancreas (the head of the pancreas), and the pancreas. The stomach, liver, spleen, small intestine, gallbladder, major blood arteries, etc. surround the pancreas as an organ. Anatomically, it is separated into three parts: the head (broad portion), neck or body (midsection), and tail (thin portion). In order to digest meals and control blood sugar levels, the pancreas secretes hormones (insulin and glucagon). The pancreas can develop a variety of malignant and non-cancerous tumours, which are typically limited to the head or the widest part of the organ and are treated using the Whipple technique.
Surgery for tumours or disorders in the body and tail of the pancreas
Distal pancreatectomy is used to treat benign or malignant tumours that are detected in the body and tail of the pancreas. This is a surgical treatment in which the duodenum and the bile duct are left unaffected and just the afflicted body and tail of the pancreas are removed. The spleen may or may not be removed during a plenectomy. While benign tumours leave the spleen intact, malignant pancreatic tumours typically necessitate splenectomy. Laparoscopic distal pancreatectomy is a minimally invasive strategy that uses a single, larger incision to perform the treatment. This method has fewer risks, a shorter hospital stay, and faster recovery times than open distal pancreatectomy. In order to provide a close-up look of the pancreas and the surrounding tissues, a laparoscope is placed into one of the incisions. The afflicted pancreatic body and tail, as well as the spleen (if necessary), are all removed. The process takes between three and four hours to complete and is carried out under general anaesthesia.
Surgery for tumours affecting nearby blood vessels
The Superior Mesenteric Artery and Superior Mesenteric Vein are two significant blood arteries that are close to the location of the pancreas. Borderline resectable pancreatic cancer is the term used to describe pancreatic cancer that has progressed to these significant blood vessels. Chemotherapy, surgery, or a combination of the two may be used as treatment at this stage, depending on the blood vessel damaged and the cancer's spread. Pancreatic cancer may first undergo chemotherapy and radiation (chemoradiotherapy) to decrease the malignant mass before being surgically removed if it is too close to or around a major artery or vein. A separate method known as palliative surgery or bypass surgery, which includes removing and reconstructing specific blood vessel segments, is occasionally performed to assist in reducing symptoms during surgery when the surgeon understands that the cancer has progressed too far and may not be able to be removed. Chemotherapy may be used following surgery to lower the risk of cancer recurrence. Visit our Liver Hospital in India for the best treatments.
Why is a Whipple procedure done
It is also known as a pancreaticoduodenectomy, and is used to treat pancreatic cancer as well as other diseases and abnormalities of the pancreas, bile duct, duodenum, and other organs. The pancreas is positioned between the stomach, liver, spleen, small intestine, gallbladder, main blood vessels, etc. It releases hormones (insulin and glucagon) to control blood sugar levels as well as digestive enzymes to break down food. The following conditions may benefit from a Whipple procedure:
Cancer of the pancreas, bile ducts, duodenum, etc.
Tumour growth in the pancreas, neuroendocrine glands, small intestine, etc.
Pancreatic cysts
Chronic pancreatitis
Ampullary cancer
Trauma to the pancreas or duodenum
Risks
When carried out by surgeons with exceptional training and expertise, the Whipple procedure is a complicated operation and has a lower incidence of complications. Following surgery, there are some risks that include:
Bleeding near the location of the incision or inside the abdomen
Infection of the abdominal cavity and the site of the incision.
Eating challenges brought on by a delay in stomach emptying.
Discharge or leaking from the bile duct connection or pancreatic
Following surgery, penumonia
Diabetes
Cancer recurrence
Preparation
Before the treatment, a number of things are examined to choose the best course of action for your circumstances. Your health issues may be maintained along with tests and scans to stage the cancer and determine whether it has progressed outside the pancreas. Your doctor will go over what to expect during the procedure and will give you instructions on how to care for yourself before and after. Before the surgery, you will be advised to start chest physical therapy, which reduces post-operative chest issues. Laparoscopic or robotic surgeries are examples of less invasive procedures that can be used to do a Whipple procedure. Less blood loss, a quicker recovery, fewer problems, and other advantages are provided by minimally invasive procedures.
Open surgery is carried out through an abdominal midline incision. Before removing the tumour, the abdominal cavity is thoroughly examined to make sure the tumour has not spread to the adjacent tissues.
In order to do laparoscopic surgery, which is a minimally invasive operation, your abdomen is divided into four to five smaller incisions. Through these incisions, specialised tools and laparoscopy are inserted to eliminate the tumour development.
Sophisticated surgical tools are mounted on a robotic arm to perform robotic surgery, which is a minimally invasive operation. While performing the procedure, the robotic arm can simulate a human hand. The surgeon operates by guiding the robotic arm with hand controls while commanding it from a console nearby.
Food and Medications
Talk to your doctor about your worries. Inform the doctor about all of the medications and supplements you are taking, as well as any allergies you may have to any specific drugs, anaesthesia, etc. You can discuss your dietary limitations with your doctor, as well as if you can take drugs both before and after the treatment. Nevertheless, you might be asked to cease taking blood-thinning medicine a week prior to the treatment and fast for around 8 hours beforehand. Book an appointment at Manipal Hospitals for the best Whipple surgery treatment in India.
Before the procedure
You'll be asked to change into a surgical gown on the day of the surgery, and your abdomen will be cleaned, draped, and treated with an antiseptic. Through the intravenous (IV) line that is implanted in your arm, fluid and medications are administered. These drugs will keep you from getting sick and relax you. Your bladder will be punctured to place a urinary catheter, which will drain and collect urine both during and after the operation. An epidural catheter or spinal injection is given to lessen post-operative pain and suffering and to use fewer narcotic pain medicines.
During the procedure
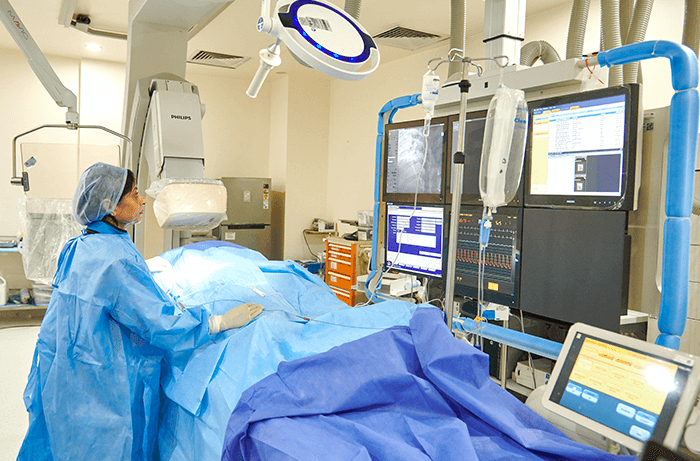
This intricate procedure is carried out by a group of highly qualified and experienced pancreatic surgeons, nurses, technicians, anaesthetists, etc., and can last anywhere from 4 to 12 hours. You receive general anaesthesia, and throughout the procedure, your vital signs are continuously checked. The pancreas and other organs are accessed via a midline incision (open surgery) or many small incisions (laparoscopic or robotic surgery) on the belly, depending on the chosen strategy. To ensure that the tumour has not spread to the neighbouring organs and tissues, the internal organs are carefully examined. The bile duct, gallbladder, duodenum, and head of the pancreas are all removed. A typical Whipple treatment, in which a portion of the stomach or the surrounding lymph nodes are removed, is occasionally performed. Pylorus preservation Whipple procedures are also sometimes used. Reconstruction begins after the area of the pancreas containing the tumour and its surrounding structures has been removed. The bile duct, intestine, and stomach are rejoined or anastomosed to the remaining portion of the healthy pancreas.
After procedure
You will spend a few days being observed in an ICU unit after the procedure. The nursing staff will keep a close eye on your development and look out for any infections or issues. The nasogastric tube is withdrawn the day after surgery, and the urine catheter is removed a few days later. You'll be forced to walk slowly with help. A few sips of water will be permitted, and your diet will gradually transition from liquids to soft meals and then to a regular, palatable diet. You might stay in the hospital for a week, depending on how quickly the incision heals and any post-operative complications. Before a patient is ready to be discharged, they typically need to spend 1-2 days in the ICU and 5–6 days in the ward. You will be able to lead a normal life once the recuperation phase has passed for a few weeks. The resected specimen is sent for histopathology (biopsy) analysis following the operation, which results in the final stage of the tumour. The pathologist looks at the sample under a microscope before giving the tumour a clinical stage. The patient's long-term prognosis is based on the pathological stage of the tumour. It also establishes whether the patient needs additional radiotherapy or chemotherapy to prevent the cancer from returning. If chemotherapy and radiation therapy are necessary, they are scheduled a few weeks after the patient has fully recovered from the operation.