×
Select Your Country
 International
International

×
Select Your Country
 International
International

What is TAVR?
Also known as the Transcatheter aortic valve implantation (TAVI), the TAVR is a minimally invasive procedure that involves inserting or placing a new valve inside the damaged or diseased heart valve. In this procedure, the old valve is not removed. After the new valve has been placed inside the old and damaged valve, it expands, thus pushing the leaflets of the old valve out of the way.
Why is the procedure recommended?
The procedure is recommended for patients with intermediate-risk of aortic stenosis. Aortic stenosis involves the narrowing of the aortic valve, which restricts the flow of blood from the left ventricle to the aorta. Severe aortic stenosis occurs because of congenital heart defects (bicuspid aortic valve) or ageing as calcium deposits and plaque can damage the heart valve and prevent it from fully opening. Some of the major symptoms of aortic stenosis are palpitation, chest pain, dizziness, shortness of breath, fatigue even after walking for a short distance, and difficulty in falling asleep. These symptoms usually occur when the blood flow is considerably reduced. Hence, it is necessary to visit a doctor even if there is a slight reduction in your energy and you find performing routine activities and tasks difficult because of fatigue. High-risk patients who are not fit for the surgical valve replacement (SAVR) procedure and are inoperable are also advised to undergo this procedure.
How is it performed?
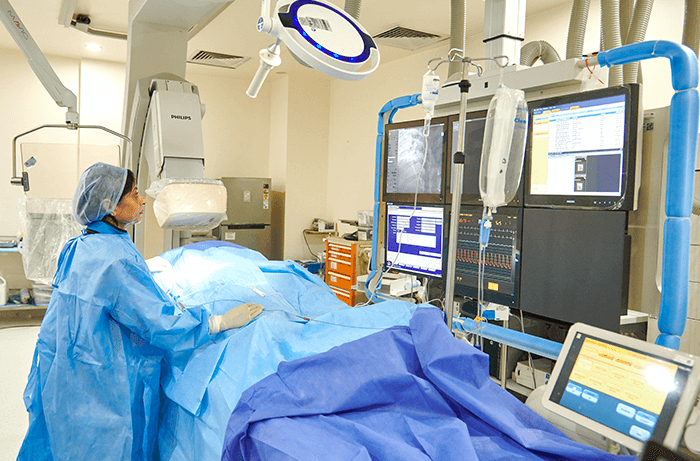
General anaesthesia is used while performing the TAVR procedure. Vitals, such as heart functions, heart rhythm, and blood pressure, are constantly monitored throughout the procedure. There are mainly two approaches that are adopted by surgeons or cardiologists for accessing the heart valve:
Transfemoral approach: In this approach, a small incision is made in the groin for creating an opening in the femoral artery. In this method, no incision is made in the chest.
Transapical approach: This approach involves making a small incision in the chest for creating an opening in the large artery.
After selecting the safest approach, a guidewire is introduced via a flexible tube called an introducer sheath. This is followed by the passing of a flexible tube called a catheter, which is connected with a balloon, through the guidewire and right into the aortic valve. For guiding the catheter into the aorta, advanced imaging techniques are used. To widen the aortic valve, an inflated balloon is utilized, which is deflated after the valve has been widened and moved towards the sides. The retraction of the catheter follows this. Another catheter is then fitted with a balloon and a folded prosthetic new heart valve, which is covered with a wire mesh (stent), is inserted into the aorta. After the insertion of the new valve inside the old, damaged valve, the balloon expands, which pushes the old valve leaflets out of the way. This is followed by the removal of the catheter along with the guidewire and the closing and dressing of the incision.
Advantages of the TAVR Procedure:
It is a safe and effective procedure and can provide relief from the symptoms of severe aortic valve stenosis.
The patient feels less anxious, more energetic, and can breathe normally after undergoing the surgery.
It massively improves the chances of survival for patients with severe symptoms.
It doesn’t cause any trauma to the ribs, heart muscles, and breastbone and significant blood loss. Moreover, the chances of infection are quite low in this procedure.
The risk of vascular injury is considerably low because of improved transcatheter design.
Due to the adoption of better transcatheter design and advanced imaging technology, the procedure causes fewer complications, such as paravalvular leakages and stroke.
Who Benefits from the Procedure?
The procedure is beneficial for:
Patients diagnosed with aortic stenosis and suffering from chest pain, shortness of breath, swelling of the leg, and fatigue.
Patients who are highly vulnerable to complications arising from open-heart surgeries or surgical aortic valve replacement (SAVR) procedures.
Patients who are inoperable due to age and other comorbidities.
Patients who are implanted with a biological tissue valve that has failed to work effectively.
Risks of Undergoing the Procedure
If the prosthetic valve used for replacement in the procedure is not of the correct size or doesn’t fully expand, blood may leak from it.
This procedure is sometimes associated with vascular access-site complications, which primarily occur because of a mismatch between the sheaths of the delivery system and the access artery on account of the calcification of the access artery or due to the larger diameter of the delivery system.
The procedure can sometimes cause the device landing-zone to rupture because of ventricular outflow tract calcifications, severe annular, or aggressive over-sized prosthetic valve.
Aortic valve regurgitation: The improper placement of the prosthetic valve or size mismatch of the prosthetic valve-annulus cause paravalvular leak while severe or moderate central leak occurs because of dysfunction in the valve’s structure.
The mispositioning of the prosthetic valve can sometimes occur because of the incorrect assessment of the aortic annulus or the incorrect implantation of the prosthetic valve.
The procedure is also associated with coronary obstruction, which generally occurs because of the excessive calcification of the aortic valve’s leaflets and the aggressively oversized prosthetic valve.
The procedure can sometimes cause cerebrovascular complications.
The patients undergoing the procedure can suffer from cardiac conduction abnormalities.
In some cases, the implantation of a permanent pacemaker is required.
The contrast dye utilized for imaging can cause damage to the kidneys, but this is highly uncommon and usually reversible.
The risk of myocardial infarction is quite high in these procedures.
The likelihood of stroke is considerably high.
Patients may suffer from excessive bleeding.
Very sick patients or those with comorbidities may not survive the procedure sometimes but this is generally very rare.
How is the Procedure Different from Standard Valve Replacement?
Open-heart surgery is conducted during a standard valve replacement procedure, in which, the chest wall (sternotomy) and heart muscles are cut open with the help of a larger incision for accessing the heart valve. The heart is temporarily stopped and a heart-bypass machine is used for pumping blood. Whereas, the Transcatheter Aortic Valve Replacement (TAVR) procedure in India is conducted via small openings and it is less invasive, which helps spare the ribcage and breastbone. In addition, the recovery time of the patient post-TAVR is less than that post-standard valve replacement.
Things to Expect Pre-Procedure and Post-Procedure
Pre- Procedure:
The doctor must be notified about the supplements and medicines that the patient is taking.
The patient must schedule an appointment with a dentist to ensure that they don’t have any infection in the teeth or mouth as it can spread to the heart.
The patient must not take any blood thinner or other medicines around 2 weeks before the procedure to mitigate the chances of bleeding.
The patient must immediately notify the doctor if they have a fever, cold, herpes etc.
The patient must stop drinking alcohol and smoking.
Post-Procedure:
The patient will be shifted to the intensive care unit (ICU) and their vitals will be monitored continuously for the following 24 hours.
The patient might have to spend a couple of days at the hospital.
The patient will be expected to move and walk around to strengthen their body and heart.
The patient will be taught a few simple exercises and self-care methods including the correct way to take a shower and care for the wound.
A heart-healthy diet will be given to the patient.
The patient will be prescribed certain blood-thinning medicines and painkillers.
The patient is advised to visit the hospital regularly for follow-up appointments with the cardiovascular surgeon in India.
As the procedure is minimally invasive and involves small incisions on the body, the patient will be expected to stay in the hospital for around 2-5 days and after 4-6 weeks after the procedure, they will have to visit the hospital for follow-up appointments with the doctor.
The durability of the valve depends on the type of prosthetic valve used, the patient’s age, and medical condition. A mechanical valve is generally provided to younger patients and it can last for the rest of the patient’s life. However, it necessitates the lifelong use of anticoagulants. On the other hand, a biological prosthetic valve is vulnerable to structural valve deterioration and can last for 5-10 years with proper care. The valves implanted in younger patients usually last for around 5 years as these patients generally have active lifestyles.
Patients usually suffer from pains and aches in the incision site after the procedure. The pain is expected to subside after some time. However, the patient has still been prescribed painkillers as it speeds up the healing process. The patient is advised to follow the instructions of the doctor for follow-up diet, exercises, and care. It usually takes a patient 6-10 weeks to recover fully. Moreover, it is easier to recover from a TAVR than open-heart surgery.
TAVR has increased the life expectancy of extreme-risk patients, who are above the age of 80 years, have comorbidities, and cannot tolerate open-heart procedures, to nearly 30 months from 11 months. We are still awaiting the results of long-term studies on the life expectancy of moderate- and low-risk patients after a TAVR procedure.