×
Select Your Country
 International
International

×
Select Your Country
 International
International


Millions of people around the world have sickle cell disease (SCD), which is a global health problem. It is a genetic blood disorder that can make life very hard and cause severe symptoms. Sickle cell disease (SCD) is common, but many people don't know much about it. The uncertainty makes it challenging to get a diagnosis, get the right treatment, and find the support networks that people with the disease need.
Sickle cell disease is a genetic blood disorder that affects the way haemoglobin, the protein in red blood cells that carries oxygen around the body, works. Red blood cells are flexible, disc-shaped, and can easily move through blood vessels in healthy people.
People who have sickle cell disease have a genetic change that causes their bodies to make sickle haemoglobin, which is also known as haemoglobin S. For example, when oxygen levels are low or the body is dehydrated, red blood cells become stiff and take on a crescent or "sickle" shape.
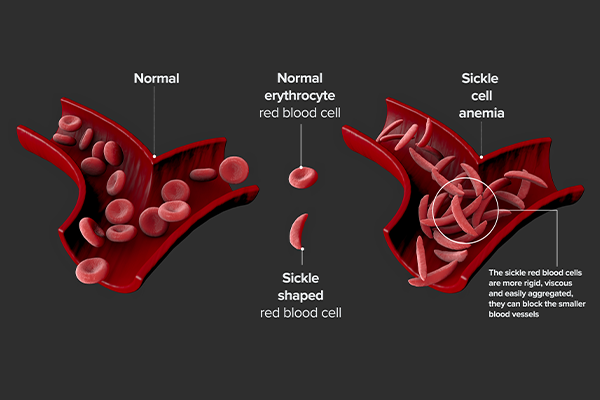
There are a few reasons why these sickle-shaped cells are bad:
Stiffness: Sickle cells are stiff and can get stuck in small blood vessels, which is not the case with healthy, flexible red blood cells.
Weakness: Sickle cells are more likely to break down before they should than normal red blood cells. This leads to chronic anaemia.
Short Lifespan: Healthy red blood cells can live for up to 120 days, but sickle cells only live for 10 to 20 days.
Sickle cell disease is caused by genetics; it is an autosomal recessive genetic disorder. This means that a person needs to get two copies of the bad gene, one from each parent, to get the disease.
Sickle Cell Trait (SCT): If you have one copy of the sickle cell gene and one copy of the normal haemoglobin gene, you have sickle cell trait. People with SCT don't usually have the same symptoms as people with SCD. But in very rare and extreme cases, like when they do a lot of physical activity at high altitudes, they might have some trouble. It is very important that people with SCT can pass the gene on to their children.
Sickle Cell Disease: If both parents have the sickle cell trait, there is a 25% chance that their child will inherit two copies of the abnormal gene and get SCD. The child has a 50% chance of inheriting one copy of the gene and having the trait, and a 25% chance of inheriting two normal genes.
People with a family history of SCD or couples who want to start a family and are worried about their carrier status should strongly consider genetic counselling.
Here's a table summarising the types of sickle cell disease :
| Type of Sickle Cell Disease | Severity | Key Characteristics |
| HbSS (Sickle Cell Anemia) | Most severe | The most common type is HbSS. Individuals typically experience the most significant symptoms and complications associated with sickle cell disease. |
| HbSC Disease | Generally less severe than HbSS | While typically milder than HbSS, individuals can still experience serious complications. |
| HbS Beta-Thalassemia | Varies: HbS beta-plus is less severe; HbS beta-zero is more severe (similar to HbSS). | This type has two main subtypes, with varying levels of severity depending on whether it's beta-plus or beta-zero thalassaemia. |
| HbSD, HbSE, HbSO-Arab | Varies widely based on a specific combination | These are less common types, and the severity of the disease can differ significantly depending on the particular abnormal haemoglobin gene inherited alongside HbS. |
Sickle cells, shaped and functioning differently from normal cells, cause Sickle Cell Disease (SCD). These are sickle cell disease symptoms and problems. These can be very different in how detrimental they are for each person.
Some common sickle cell disease symptoms are:
Anaemia: Chronic anaemia is a common sign of SCD because sickle cells die faster than they are made. This disorder can make you exhausted, out of breath, dizzy, and have pale skin.
Pain Crises (Vaso-occlusive Crises): This type of syndrome is one of the most common and painful symptoms. When sickle cells block small blood vessels, they cut off oxygen-rich blood to tissues and organs, which causes a lot of pain. These crises can These conditions can occur anywhere in the body, but they are most commonly found in the chest, abdomen, and bones. The severity and frequency of pain crises can vary significantly.
Swelling of the hands and feet (dactylitis) is often one of the first signs of SCD in babies. Painful swelling happens when blood can't get to the hands and feet.
Frequent Infections: SCD patients are more prone to bacterial infections, especially as children, due to spleen damage.
Delayed Growth and Puberty: Chronic anaemia and the body's higher energy needs because of SCD can cause growth and development to be slower.
Problems with vision: When blood vessels in the eyes get blocked, they can hurt the retina and even cause vision loss.
Acute Chest Syndrome (ACS) is a serious complication that can kill you. It causes chest pain, fever, and trouble breathing. It can be caused by an infection or by sickle cells blocking blood vessels in the lungs.
Stroke: Sickle cells can block blood vessels in the brain, which can lead to stroke and serious damage to the nervous system. This is especially worrying for kids.
Damage to organs: Over time, repeated blockages and lack of oxygen can hurt different organs, such as the heart, liver, and kidneys.
Leg ulcers are open sores that occur on the lower legs due to poor circulation.
Gallstones: Bilirubin is made when red blood cells break down quickly, which can cause gallstones to form.
Early diagnosis is essential for effective management and to avoid problems, especially in babies.
Newborn screening: In a lot of places, newborn screening programs use a blood sample to check for SCD shortly after birth. This makes it possible for families to get help and learn early on.
Blood Tests: A haemoglobin electrophoresis test can find abnormal haemoglobin S in older kids and adults.
Genetic testing can help confirm the diagnosis and find out if someone is a carrier.
There is not yet a universal cure for SCD, but improvements in medical care have changed the lives of many people with the condition, letting them live longer and happier lives. Sickle cell disease treatments aim to stop complications, control symptoms, and make life better.
Important Parts of Management Are:
Pain management is a key part of SCD care. It includes both over-the-counter painkillers for mild pain and stronger prescription drugs, like opioids, for severe pain attacks. During times of pain, it's also critical to stay hydrated.
Hydroxyurea is a drug that is thought to change the course of sickle cell disease. It works by making more foetal haemoglobin (Haemoglobin F), which stops red blood cells from sickling. Hydroxyurea can help lower the number of pain crises, acute chest syndrome, and blood transfusions that are needed.
Blood transfusions: Children who are at high risk of having a stroke or who have severe anaemia or other problems get regular blood transfusions to keep them from having one.
Infection Prevention: People with SCD are more likely to get infections, so they get regular vaccinations and often take penicillin every day, especially when they are young, to avoid serious bacterial infections.
Bone Marrow Transplant (Stem Cell Transplant): This form of therapy is the only way to cure SCD that we know of right now. But it's a complicated procedure with many risks, and it needs a donor who is a good match (usually a sibling). It's usually only used for extreme cases or cases with certain problems.
Sickle Cell Disease is a very complex and hard-to-understand genetic disorder that affects millions. SCD is hard to manage, but progress has been made in understanding it. to deal with. If people with sickle cell disease are diagnosed early, get good medical care, and have strong support systems, they can live happy lives.
Reputable healthcare providers, such as Manipal Hospitals Global, are dedicated to delivering advanced treatments and facilitating research to ensure that all individuals in need receive quality care. To finally solve this global health problem and make life better for everyone with Sickle Cell Disease, we need to keep fighting for change, raise awareness, and commit to research.

Sickle cell disease (SCD) is a genetic blood disorder that changes the protein in red blood cells called haemoglobin, which carries oxygen. A genetic change causes red blood cells to be hard, brittle, and shaped like a crescent or "sickle". These cells don't live as long (10 to 20 days instead of 120 days for healthy cells), which makes you chronically anaemic. They can also get stuck in small blood vessels, which stops blood from flowing.
Sickle cell disease is a genetic condition that is inherited through autosomes. This means that a person needs to get two copies of the harmful gene, one from each parent, to get the disease. If both parents have the sickle cell trait (meaning they have one normal gene and one sickle cell gene), there is a 25% chance that their child will be born with sickle cell disease.
The sickle-shaped cells stop blood from flowing and make it difficult for the body to get oxygen, which causes the symptoms and problems. The most common and debilitating symptom is a pain crisis (or vaso-occlusive crisis).
These episodes are characterised by severe pain. Some other common signs and serious problems are:
Long-lasting anaemia that makes you tired and dizzy
Dactylitis, or swelling of the hands and feet, is common in babies.
A damaged spleen makes you more likely to get infections.
Acute Chest Syndrome is a lung disease that can kill you.
Kids are more likely to have a stroke if they are older.
Long-term damage to the kidneys, liver, and heart
There is no universal cure yet, but treatment aims to control symptoms, avoid complications, and make life better. Some important ways to manage are:
Pain management includes drinking enough fluids and taking various medicines, from over-the-counter painkillers to strong prescription drugs for very bad pain.
Hydroxyurea is a medicine that stops sickle cells from forming. This makes pain crises and other problems less common.
We give blood transfusions to people with severe anaemia and to kids who are at high risk of having a stroke.
Young kids especially need to take antibiotics every day (like penicillin) and get their shots on a regular basis to stay healthy.
The only way to cure sickle cell disease right now is with a bone marrow transplant (or stem cell transplant). But this is a complicated and risky procedure that only happens in very rare cases and usually needs a sibling as a donor. Gene therapy and gene-editing technologies are two new treatments that are being tested in clinical trials right now. They could be the way to cure this disease in the future.