Welcoming a new baby is pure magic—but let’s be real, it also brings a wave of questions, especially around breastfeeding. Is this normal? Am I doing it right? Why is no one talking about this part? If you’re nodding along, you’re in the right place.
Based on real-world experience with new mums just like you, this blog offers clear, practical breastfeeding tips to help you feel more confident and less overwhelmed. Take a deep breath—you’ve got this.
1. How often does my newborn really need to breastfeed?
Trust your baby, not the clock. In the early days, newborns usually want to feed every 1.5 to 3 hours. Some days it feels constant—this is how your baby builds your milk supply and feels secure. Instead of watching the time, follow your baby's hunger cues: rooting, lip smacking, and hands to mouth. Crying is a late sign—feeding earlier can help both of you stay calmer and more content.
Watch for output, not just input. It’s easy to worry whether your baby is getting enough milk, especially when feeds feel short or irregular. Rather than tracking minutes or ounces, keep an eye on wet and dirty nappies. Plenty of pees and poos, along with steady weight gain and a content baby post-feed, are great signs things are going well.
2. How to Know if Your Baby is Getting Enough Milk: Key Signs to Watch?
Worried your baby isn't getting enough milk? It's completely normal for new parents to wonder! Here’s what you can look for—no need to guess or compare with anyone else.
1. Wet Diaper Count
A baby might wet at least 3-8 wet diapers a day after the first few days of life. This is one of the happiest signs that your baby is drinking well.
2. Steady Weight Gain
Your baby should steadily gain weight after the first week. Don't panic over small fluctuations—it's the overall trend that matters.
3. Baby’s Behavior After Feeding
A baby who’s getting enough milk will often be calm, relaxed, and seem satisfied after feeding. If your little one is content and happy, you’re on the right track.
4. Poop Pointers: What’s Normal?
-
Poop colour and texture change during the first days:
-
Days 1-2: Expect dark greenish-black, sticky stools (meconium).
-
Day 3-4: Stools become greenish, then transition to looser, yellowish, and sometimes “seedy” poop by day 5.
-
Breastfed babies often produce yellow, mustardy, or seedy stools—totally normal and a sign that they’re getting plenty of milk!
Stay tuned in to your baby rather than outside comparisons, and reach out to a paediatrician or lactation consultant if you need extra reassurance.
3. What does a good latch feel like—and why does it matter?
A good latch feels like a strong, tugging pull, not a pinch or bite. You may feel gentle stretching or a pulling sensation, but it should not hurt beyond mild tenderness in the early days.
Your baby’s mouth should open wide, covering as much of the areola (the darker area around your nipple) as possible—not just the nipple itself.
Signs your baby is latched well include:
-
Chin touching the breast.
-
Lips flared outwards (like “fish lips”).
-
Tongue cupping the breast.
-
You hear gentle swallowing, not smacking or clicking sounds.
If it hurts more than mild tenderness, gently pause, break the seal with your finger, and try latching again—pain is your body’s signal that an adjustment is needed.
4. Is breastfeeding normally painful?
Breastfeeding is NOT supposed to be painful. Mild sensitivity is common at first, but ongoing or sharp pain is a red flag. Persistent pain often means the latch or positioning needs tweaking.
Don’t “tough it out”—ask for support from a lactation consultant or healthcare provider. Even small changes can make a big difference, and feeding should quickly become comfortable.
5. What if my milk supply seems low?
Nearly every mom has a "Do I have enough milk?" moment—take a deep breath, because true low supply is rarer than it feels! Most of the time, your body knows what your baby needs. Here’s how to give your milk supply a natural boost:
-
Feed, feed, feed: Nurse your baby frequently day and night. The more your baby nurses, the more milk your body makes—supply is all about demand.
-
Go skin-to-skin: Lots of cuddles and bare-chested snuggles help trigger your milk-making hormones and calm you both.
-
Try gentle breast massage: Massaging before or during feeds can help with milk flow and letdown.
-
Fuel yourself: Ignore the dieting buzz—breastfeeding needs extra calories, not restrictions! Eat well, skip dieting, and enjoy a variety of foods.
-
Drink up: Aim for 3-4 litres of water daily; think of it as topping off your own tank so you can top off baby’s.
If your baby always seems hungry, never looks satisfied, or you’re worried about weight gain, don’t go it alone—reach out to a lactation consultant or your healthcare provider for a personalized check-in.
Pro tip: Don’t stress over pumping numbers or compare yourself to someone else. You—and your baby—are unique!
6. When should I start pumping and how do I store breast milk safely?
Pump milk only when you really need to. Over-pumping can sometimes do more harm than good by confusing your milk supply signals. When in doubt, always check with a lactation expert—they can guide you just right.
Cool facts about breast milk storage:
-
Fresh breast milk keeps for up to 4 days in the fridge when stored at the back (not the door).
-
You can freeze milk for up to 12 months in a deep freezer, but using it within 6 months is ideal for the best quality.
-
Pumping in the morning often brings more milk, but don’t stress about the volume—even small amounts add up.
If feeding is going well, give yourself about four weeks before starting to pump—unless separation for work or medical reasons calls for it. Trust your body, take it step-by-step, and remember: every little bit you pump is a win.
If you ever feel unsure, a quick chat with a pro can settle any worries!
7. Can anything in my diet boost milk supply?
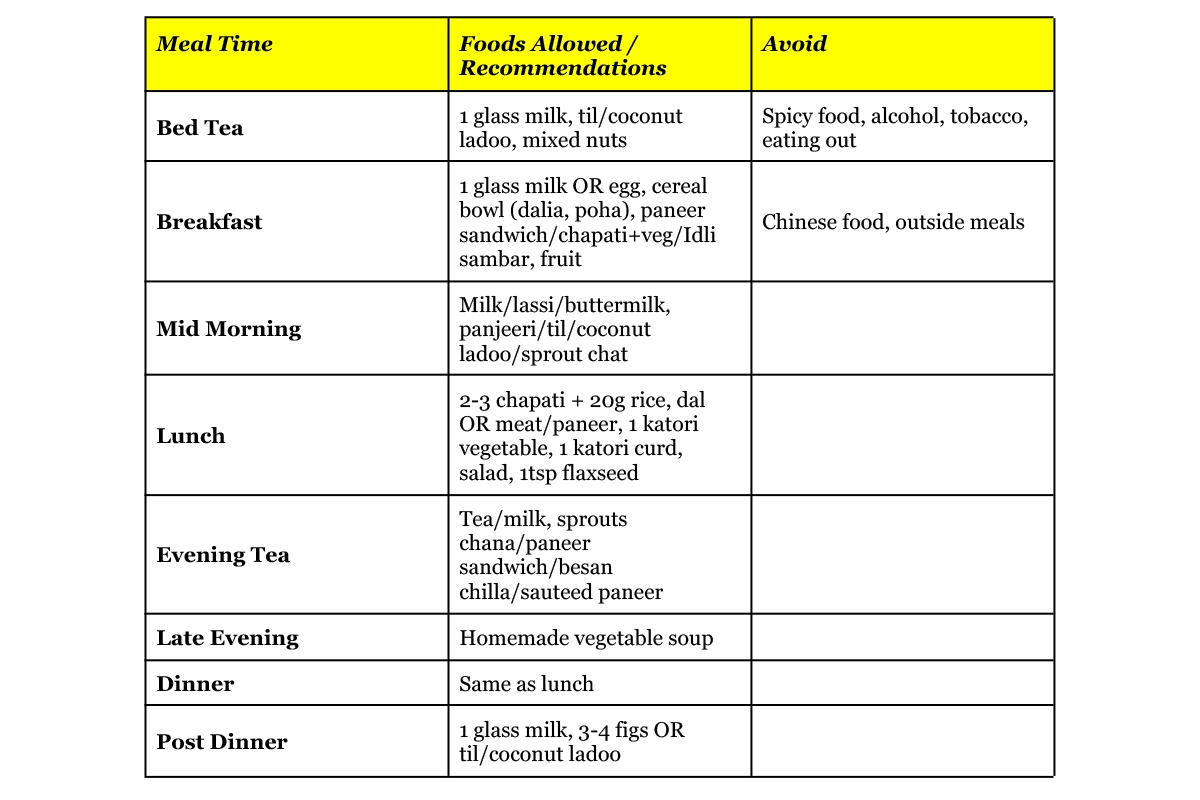
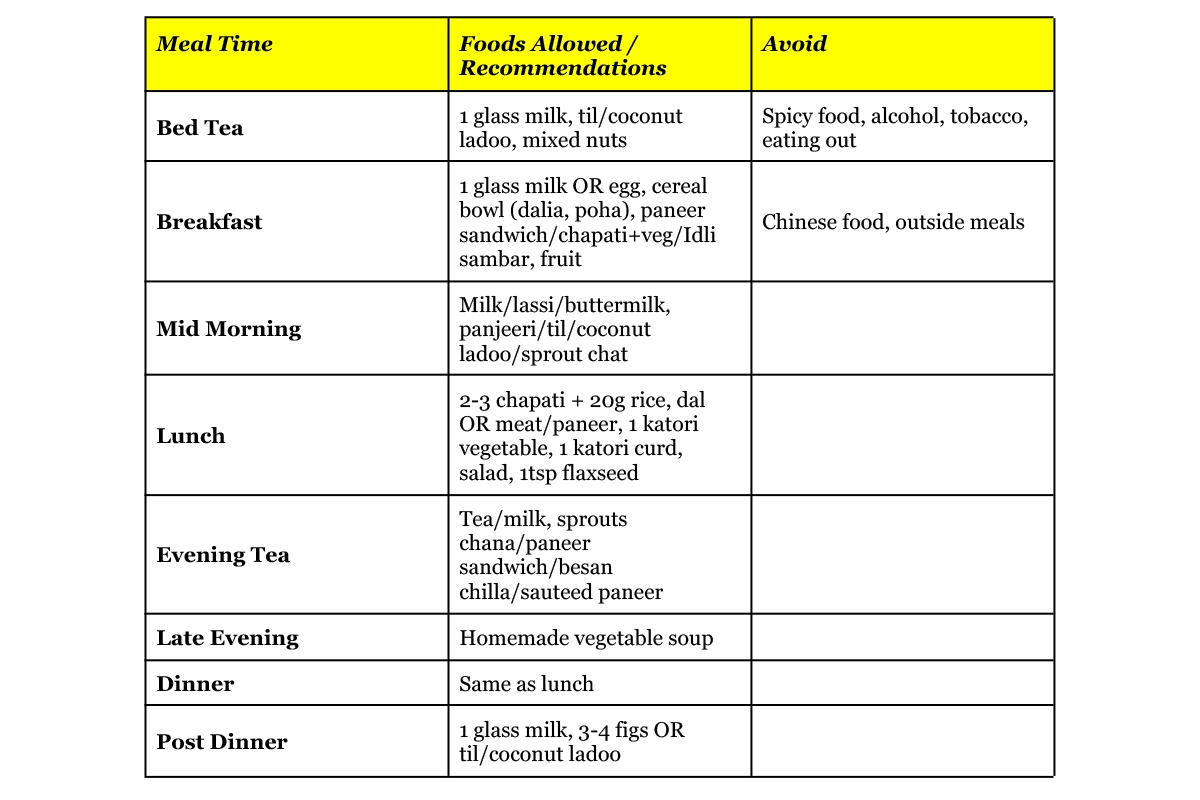
A balanced, varied home-cooked diet—rich in milk, pulses, greens, seasonal fruits, nuts, and whole grains—supports both you and your baby during lactation. Avoid excess spice, alcohol, tobacco, and outside food. No food will magically increase supply, but regular, nourishing meals, enough fluids, and self-care make all the difference.
 8. How do I prevent cracked/sore nipples?
8. How do I prevent cracked/sore nipples?
Want to keep those nursing days smooth and pain-free? Here’s how to prevent cracked and sore nipples—and yes, you can skip the obsessive cleaning! Your body is smart: it naturally releases sebum (an oily moisturiser) from glands on your nipples, keeping skin soft and shielded. Overwashing? That just strips this natural balm away, making irritation and cracking more likely.
Quick Tips for Happy, Healthy Nipples
-
Ditch the constant soap and scrubbing—just gentle rinsing with warm water is all you need. Let your skin’s own moisture do the work.
-
Ensure a deep latch every feed; it’s the best defence against soreness.
-
Mix up your breastfeeding positions to spread out any pressure.
-
Air-dry nipples after feeding—or smooth on a few drops of your own breast milk for an extra healing boost.
-
Skip harsh soaps, scents, or sprays on your breasts.
-
Wear soft, loose cotton bras for maximum comfort and breathability.
-
If soreness sneaks in, don’t wait—connect with a lactation consultant if things don’t improve quickly.
9. What are the real benefits of breastfeeding for me and my baby?
Breastfeeding is truly a win-win for both you and your baby—here’s why:
Real Benefits for Your Baby:
Built-in Immunity: Breast milk is packed with antibodies that protect your baby from infections like respiratory illnesses, diarrhoea, and ear infections, giving them a strong immune head start.
Smart Start: Studies show babies who are breastfed tend to have better brain development and score higher on IQ tests later in childhood.
Lower Risks: Breastfed babies face less risk of asthma, obesity, type 1 diabetes, and sudden infant death syndrome (SIDS).
Postpartum Healing: Breastfeeding releases hormones like oxytocin that help your uterus shrink back to its pre-pregnancy size and reduce postpartum bleeding.
Cancer Protection: Every feed lowers your future risk of breast and ovarian cancers—a powerful health shield over time.
Weight Management: Breastfeeding helps burn extra calories, assisting you in gradually returning to your pre-pregnancy weight.
Stress & Bonding: Beyond biology, breastfeeding creates quiet, tender moments—your baby’s sleepy smile, the warmth of skin-to-skin—that foster lifelong emotional connection and reduce stress for both of you.
So, beyond nourishing your baby with nature’s perfect food, breastfeeding is a holistic experience that heals, protects, and connects you in deep and lasting ways. Those tiny moments at the breast are building blocks for a healthy future—for both of you.
Conclusion
Every mother's breastfeeding journey is different, filled with challenges, doubts, and innumerable priceless moments. You deserve knowledge, support, and a caring team on your side whether you're just starting out or looking for assistance on this journey.
We at Manipal Hospitals Global think that strong, independent mums produce happy, healthy children. Every step of the way, our committed lactation consultants, skilled nurses, and top-notch maternity care team are available to answer your questions, offer solutions to your problems, and recognise your accomplishments, no matter how small. We offer the best evidence-based care in a safe, friendly environment, whether you're overcoming obstacles, navigating your first latch, or just seeking comfort.
If you ever feel confused, overwhelmed, or just wish you had a little extra support, please reach out. There’s no question it's too small. We’re here to help you and your baby flourish. Give yourself grace, celebrate the little milestones, and remember: you and your baby are learning together—and that’s more than enough.